If a dentist recommends root canal therapy, it’s understandable to feel uneasy — but there’s good reason not to panic. Modern endodontic care is predictable and focused on comfort; many patients describe the experience as comparable to receiving a routine dental filling. When a tooth’s inner tissues are infected or irreversibly damaged, root canal treatment often relieves pain and preserves the tooth so you can keep your natural smile.
At the office of SmileArts Dental, we combine up-to-date techniques with a patient-first approach to deliver careful, efficient root canal care. Our team prioritizes comfort, clear communication, and clinical precision so you understand your options and feel confident in the treatment plan.
A natural tooth offers strength, stability, and function that are difficult to fully replicate with replacement options. When possible, saving a tooth with root canal therapy maintains bite alignment, supports surrounding teeth, and preserves jawbone health. Choosing to retain a natural tooth often leads to better long-term outcomes for chewing, speech, and overall oral health.
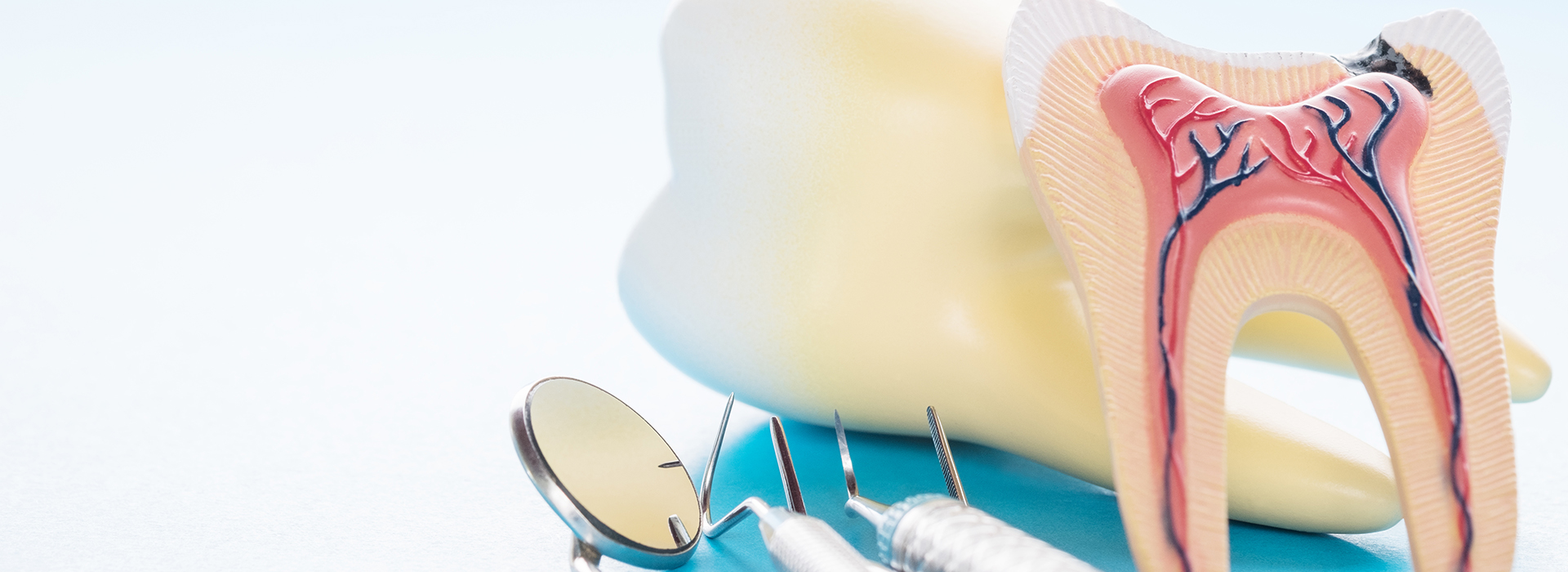
Root canal therapy removes the diseased or damaged pulp inside a tooth while leaving the outer structure intact. After the canal system is cleaned and sealed, the tooth is typically restored with a crown or other permanent restoration to protect it from fracture and restore full function. This layered approach — treating the interior first, restoring the exterior second — helps the tooth endure for many years when properly cared for.
Advances in instrumentation and materials have made endodontic procedures both more accurate and more comfortable than in the past. When performed on time and with appropriate restoration, a treated tooth can often serve reliably for the rest of a patient’s life.

At the center of each mature tooth lies the dental pulp — a soft tissue complex of nerves, blood vessels, and connective tissue. While essential during tooth development, the pulp can become inflamed or infected after deep decay, cracks, traumatic injury, or repeated dental work. When inflammation is severe or the pulp can no longer recover, the tissue may die and an infection can spread to the root tips and surrounding bone.
Symptoms vary. Some patients experience sharp, lingering pain with hot or cold, pain when biting, or swelling of the gums. Others have no symptoms at all and learn about the problem through a routine exam or X-ray that reveals changes at the root tip. Because signs can be inconsistent, a thorough clinical and radiographic evaluation is needed to identify when root canal treatment is the appropriate course.
Prompt diagnosis matters: the longer an infection persists, the greater the risk it spreads or causes more extensive bone loss. In many cases, early treatment reduces complications and preserves more of the natural tooth structure.
Although not every ache or sensitivity requires root canal therapy, watch for the following warning signs that may indicate deeper trouble:
Pain that lingers after exposure to hot or cold, or pain severe enough to interrupt sleep, often points to pulp involvement. This kind of persistent discomfort should be evaluated promptly.
Prolonged sensitivity to hot or cold — especially if the sensation becomes more painful over time — can signal that the nerve tissue is inflamed or compromised.
Discomfort with pressure, even light touch, may indicate infection or structural damage that has reached the inner tissues of the tooth.
When internal tissues break down, a tooth can take on a darker hue. This change is often a clue that the pulp has been injured or is no longer viable.
A fractured or chipped tooth can expose the pulp to bacteria or cause direct injury to the nerve, sometimes necessitating endodontic treatment to save the tooth.
Localized swelling, a pimple-like bump on the gum, or any drainage can indicate an abscessed tooth. These signs require timely evaluation to address infection and prevent spread.
Advanced infection can erode bone support and produce mobility. Treating the underlying infection often allows healing and stabilization of the tooth.

Root canal therapy today relies on precise cleaning, shaping, and sealing of the tooth’s canal system. After isolating the tooth with a rubber dam to keep it dry and free of saliva, the clinician uses small, flexible instruments and irrigation solutions to remove diseased tissue and disinfect the canals. Cone‑beam X‑rays or digital imaging may be used to confirm anatomy and treatment progress.
Most treatments are completed under local anesthesia, making the procedure comfortable for the vast majority of patients. For those who feel anxious or need additional relaxation, sedation options are available and can be discussed before treatment to ensure a calm, controlled experience.
The canals are filled with a biocompatible material and sealer to prevent reinfection. Depending on the tooth’s condition, the dentist may place a temporary filling and schedule a follow-up visit to restore the tooth permanently with a crown or other protective restoration that restores strength and function.
After treatment, it’s normal to have mild soreness as surrounding tissues heal. Over-the-counter pain relievers are usually sufficient, and discomfort typically subsides within a few days. If swelling, increasing pain, or other concerning symptoms occur, contact our office for evaluation.
Good home care is important: continue gentle brushing and flossing and avoid chewing on the treated tooth until it has been permanently restored. A temporary filling protects the canal system, but a final crown or restoration is often recommended to prevent fracture and return the tooth to full function.
With proper treatment and routine dental care, a tooth that has undergone root canal therapy can remain stable and functional for many years. Regular dental exams and timely attention to new symptoms help protect treated teeth and support lasting oral health.

Successful treatment is a partnership between clinician and patient: early detection, timely intervention, and the completion of a permanent restoration are all part of a predictable outcome. Our team will explain each step, answer your questions, and tailor the approach to your comfort and clinical needs.
If you’re experiencing dental pain, sensitivity, swelling, or notice a change in the color of a tooth, don’t delay seeking professional care. Early assessment preserves more tooth structure and reduces the chance of more complex problems later on.
At SmileArts Dental, we are committed to delivering thoughtful, evidence-based care that prioritizes comfort and long-term results. If you would like more information about root canal therapy or need an evaluation, please contact our office to speak with a team member and arrange an appointment.
Root canal therapy is a dental procedure that removes infected or irreversibly damaged pulp from inside a tooth to relieve pain and stop the spread of infection. The clinician cleans and shapes the tooth's canal system, disinfects it with irrigants, and fills the space with a biocompatible material to seal it. Afterward, the tooth is restored with a permanent restoration, often a crown, to protect it from fracture and restore function.
This treatment preserves the natural tooth structure and maintains bite alignment, which helps protect neighboring teeth and jawbone. When performed promptly and followed by an appropriate restoration, a root canal can enable a tooth to remain functional for many years. Advances in instrumentation and anesthesia have made the procedure predictable and comfortable for most patients.
You may need a root canal when the dental pulp becomes inflamed or infected due to deep decay, a crack or chip, traumatic injury, or repeated dental procedures on the same tooth. Inflammation and infection can cause persistent pain, sensitivity to temperature, swelling, or changes in tooth color, though sometimes the problem is asymptomatic and discovered on X-rays. Left untreated, an infected pulp can lead to abscess formation and bone loss around the root tip.
An evaluation that includes a clinical exam and radiographs helps determine whether root canal therapy is the best option to save the tooth. Early intervention often preserves more tooth structure and reduces the risk of more extensive treatment later. Your dentist will discuss signs, prognosis, and the recommended next steps based on the tooth's condition.
Most root canal treatments are performed under local anesthesia, which numbs the tooth and surrounding tissues so patients feel little to no pain during the procedure. Many people describe the experience as similar to having a routine filling once adequate anesthesia is achieved. Mild soreness or tenderness in the treated area is common for a few days as the surrounding tissues heal, and over-the-counter pain relievers usually control this discomfort.
If you have dental anxiety or special needs, additional comfort measures and sedation options can be discussed before treatment to make the visit more manageable. Prompt treatment of infection also tends to reduce overall pain compared with leaving the problem untreated. If you experience increasing pain, swelling, or signs of infection after treatment, contact the office for follow-up evaluation.
Root canal treatment typically begins with isolating the tooth using a rubber dam to keep the area dry and reduce contamination. After administering local anesthesia, the dentist accesses the pulp chamber, locates and negotiates the canal system with small, flexible instruments, and thoroughly disinfects the canals using irrigation solutions and antimicrobial protocols. The canals are then shaped and filled with a biocompatible material and sealer to create a long-term seal against reinfection.
Digital imaging or cone beam radiography may be used to assess canal anatomy and confirm treatment progress, especially in complex cases. A temporary filling is sometimes placed and a follow-up appointment scheduled to place a definitive restoration, such as a crown, to restore strength and function. In certain situations a referral to an endodontist is recommended for advanced anatomy or retreatment needs.
After treatment, avoid chewing on the treated tooth until it has been permanently restored to reduce the risk of fracture, especially if a temporary filling is in place. Maintain good oral hygiene by gently brushing and flossing around the tooth to support healing and reduce the chance of new decay. Use over-the-counter pain medication as directed if you have mild soreness, and apply a cold compress for swelling if recommended by your dentist.
Follow-up care is important: complete the recommended restoration, such as a crown, to protect the tooth and restore full chewing function. Keep routine dental exams and X-rays as advised so your provider can monitor healing and the long-term integrity of the treated tooth. Report any new or worsening symptoms promptly, including persistent pain, swelling, or changes in bite.
When root canal therapy is performed correctly and the tooth receives an appropriate permanent restoration, many treated teeth remain functional for decades or even a lifetime. Longevity depends on several factors including the extent of preexisting damage, the quality of the restoration, the tooth's position and function, and ongoing oral hygiene. Regular dental care and timely attention to new problems also play a major role in long-term success.
Some teeth may be more prone to fracture or recurrent infection and require additional treatment such as retreatment or a surgical procedure at the root tip. Your dentist can provide a realistic prognosis for your specific tooth based on clinical findings and radiographic assessment. Routine monitoring helps detect changes early and preserve the tooth whenever possible.
Alternatives to root canal therapy include careful monitoring, extraction, or endodontic surgery depending on the situation and prognosis. In cases where the tooth cannot be predictably saved, extraction followed by an appropriate replacement option may be recommended to restore function and prevent shifting of adjacent teeth. Watchful waiting may be appropriate in limited scenarios where symptoms are absent and radiographs show no progressive infection, but this approach requires careful follow-up.
For previously treated teeth with persistent problems, options include nonsurgical retreatment or surgical procedures such as an apicoectomy to address infection at the root tip. Your dentist will explain which choices are clinically appropriate, the expected outcomes, and any need for collaboration with a specialist. The decision balances tooth preservation, long-term function, and overall oral health.
While many root canals are successful, failure can occur if bacteria remain, a canal is missed, or a restoration allows reinfection, and signs may include recurring pain, swelling, drainage, or a persistent sinus tract near the treated tooth. Some failures are only visible on radiographs as changes at the root tip without obvious symptoms, which is why follow-up imaging and exams are important. Tooth discoloration, increased mobility, or a change in bite can also signal complications that require evaluation.
If you notice any concerning signs after root canal therapy, contact your dental provider for assessment; they may recommend retreatment, surgical management, or referral to an endodontist depending on the cause. Timely diagnosis and intervention improve the chance of saving the tooth or selecting the next best option. Regular checkups help detect issues early, before more extensive problems develop.
Yes, a range of comfort options is available to help patients remain calm and comfortable during root canal therapy, and these can be discussed during the consultation. Most treatments are completed under local anesthesia, but for patients with dental anxiety or complex needs, oral sedatives or nitrous oxide may be offered to provide additional relaxation. Your dental team will review health history and preferences to select the safest, most appropriate approach for your visit.
Staff will explain what to expect before, during, and after treatment so you feel informed and secure throughout the process. If deeper sedation is needed, the dentist will discuss referral options or coordinate care to ensure a controlled and monitored experience. Comfort-focused care supports better treatment outcomes and a more positive patient experience.
Decision-making begins with a thorough clinical exam, diagnostic imaging and a review of your overall health and treatment goals to determine the best path forward for a specific tooth. The dentist considers factors such as the amount of remaining tooth structure, the extent of infection or fracture, the tooth's strategic value in the bite, and the likelihood of predictable long-term success with root canal therapy. When complex anatomy, prior treatment failure, or surgical needs are present, referral to an endodontist is often recommended for specialized care.
The office of SmileArts Dental will discuss the expected outcomes, procedural steps and any follow-up restoration required so you understand the rationale for the recommended plan. Collaborative care and clear communication help ensure that treatment aligns with your oral health priorities and provides the best chance of preserving natural teeth. If extraction is necessary, your dentist will explain appropriate replacement options and coordinate any subsequent restorative treatment.

Ready to Experience the SmileArts Dental Difference?
We’re here to help you take the next step toward a healthier, more confident smile. Whether you’re ready to schedule an appointment or want to learn more about our services, our friendly team is ready to assist you.
Our staff is happy to answer questions about treatment options, help you schedule your visit, and provide any information you need. Give us a call or fill out our quick online form today—we can’t wait to hear from you!